By The PPH Foundation
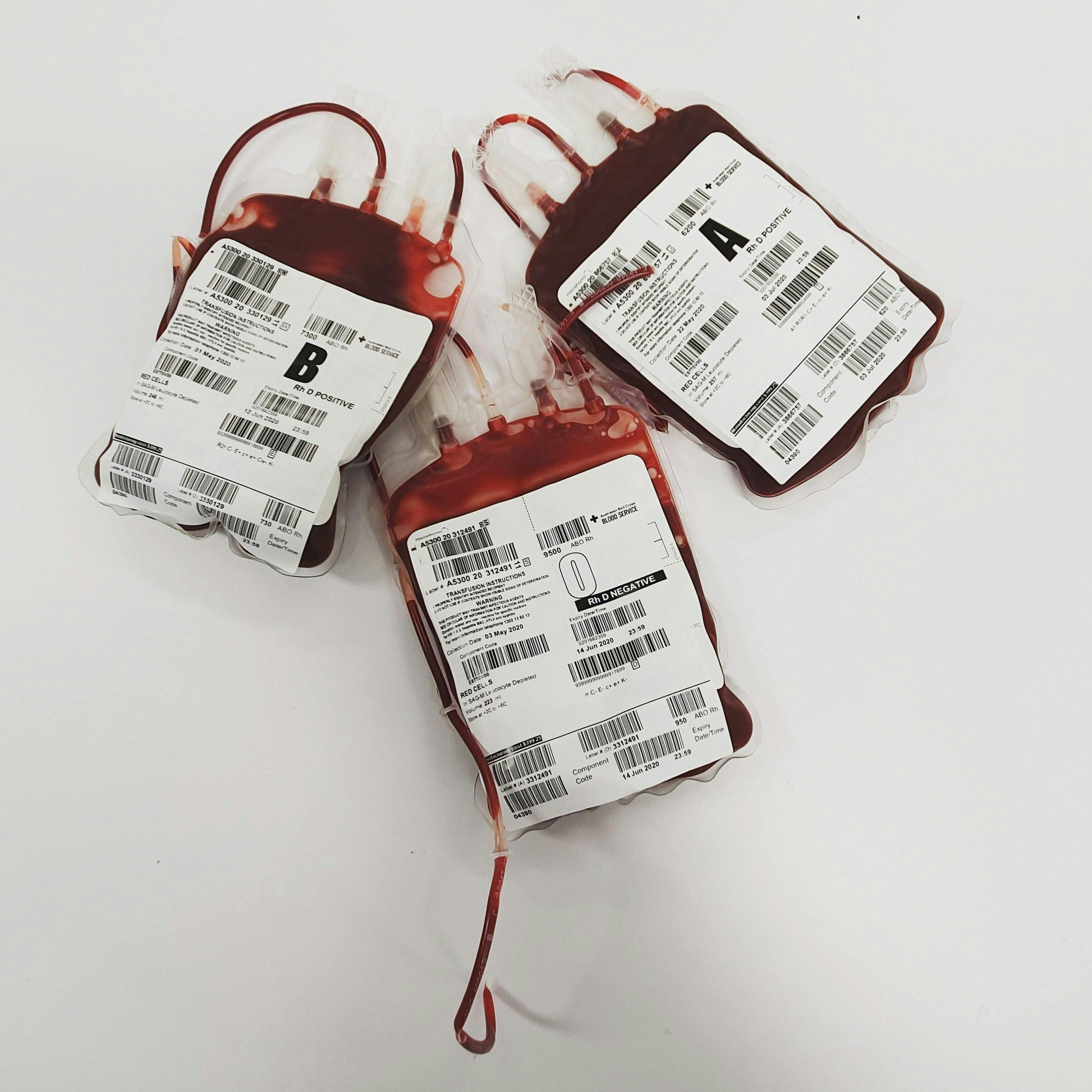
Access to safe, readily available blood is a critical pillar in the fight against postpartum haemorrhage (PPH). While prevention and rapid treatment are essential, when severe bleeding occurs after birth, a blood transfusion can literally mean the difference between life and death.
Globally, PPH remains the leading cause of maternal mortality, claiming tens of thousands of lives each year. In Kenya, experts estimate that hundreds of women die annually in health facilities because of excessive bleeding after childbirth, and one major contributing factor is a critical shortage of safe blood and efficient transfusion services. The demand for blood during obstetric emergencies such as PPH can spike sharply, and when the supply is insufficient, outcomes are often tragic.
Innovative programmes are shifting the momentum. The ROAMING Blood Typing and Acquisition Scheme, pioneered by the PPH Foundation under Prof Julius Ogeng’o, is designed to mobilise blood donors directly in communities and build a network of ready-to-respond donors. As Prof Ogeng’o said: “Roaming is anchored on the simple philosophy of bringing blood donation closer to people and building a reliable database of repeat donors.” This initiative collected nearly 875 units of blood in just ten days, demonstrating that proactive, mobile, community-based donation models can meet maternal emergency needs.
Blood matters because when PPH strikes, the uterus fails to contract (uterine atony) or there is trauma/retained placenta, causing rapid bleed-out; without restored blood volume, women become haemodynamically unstable, and organs begin to shut down within hours. Blood transfusion restores volume, improves oxygen delivery, and buys time for definitive care. Therefore, even the best prevention protocols need blood availability as a safety net.
Mobilising blood for PPH means screening donors, creating digital registries, conducting mobile drives in hard-to-reach areas, and integrating blood banks into maternal health systems. Without it, prevention fails to be fully effective, because when bleeding begins, time and volume count more than ever. Ending PPH is not only about uterotonics, monitoring, and skilled attendants; it’s also about ensuring that when bleeding strikes, blood is already waiting.
Photo by Charlie-Helen Robinson: https://www.pexels.com/photo/bags-of-blood-4531304/
Sources
- The Star (Kenya): Roaming blood initiative marks breakthrough as Kenya moves to strengthen PPH response.
- The Standard (Kenya): How “Roaming Blood” initiative seeks to rescue rural mothers.
- Nation (Kenya): Selfless lifeline, the constant donors fighting Kenya’s blood shortage.
- EndPPH.com: “ROAMING Blood Bank to Save Mothers Affected by PPH”.